Use of opioids, such as morphine and codeine, for analgesic properties dates back to antiquity. Opioid drugs have proven exquisitely powerful against moderate to severe degrees of acute and chronic pain and are today among the most commonly used analgesics in the clinic. However, while opioid drugs are instrumental in pain management, their use in some applications is hindered by a limited benefit/risk ratio. Opioid use can incur numerous side-effects (e.g. nausea/vomiting, pruritus, respiratory depression etc.), as well as addiction, the latter which is largely responsible for the dramatic rise in opioid use and overdose deaths also known as the opioid crisis. Repeated opioid use is also associated with rapid tolerance (i.e. the requirement to escalate doses to obtain equivalent analgesia). The requirement has therefore risen to search for opioid drugs with different pharmacological profiles that exploit the analgesic potential of opioid receptors while limiting the onset of associated adverse effects.
Endogenous opioid peptides and prescription opioid drugs modulate pain, anxiety and stress by activating four specific opioid receptors. However, several other receptors are also activated by endogenous opioid peptides and influence opioid-driven signalling and biology. Interestingly, these do not meet the criteria to be recognised as opioid receptors, as they are phylogenetically distant from them and are insensitive to classical non-selective opioid receptor antagonists. These atypical opioid receptors could however be used as alternative targets for the development of safer analgesics.
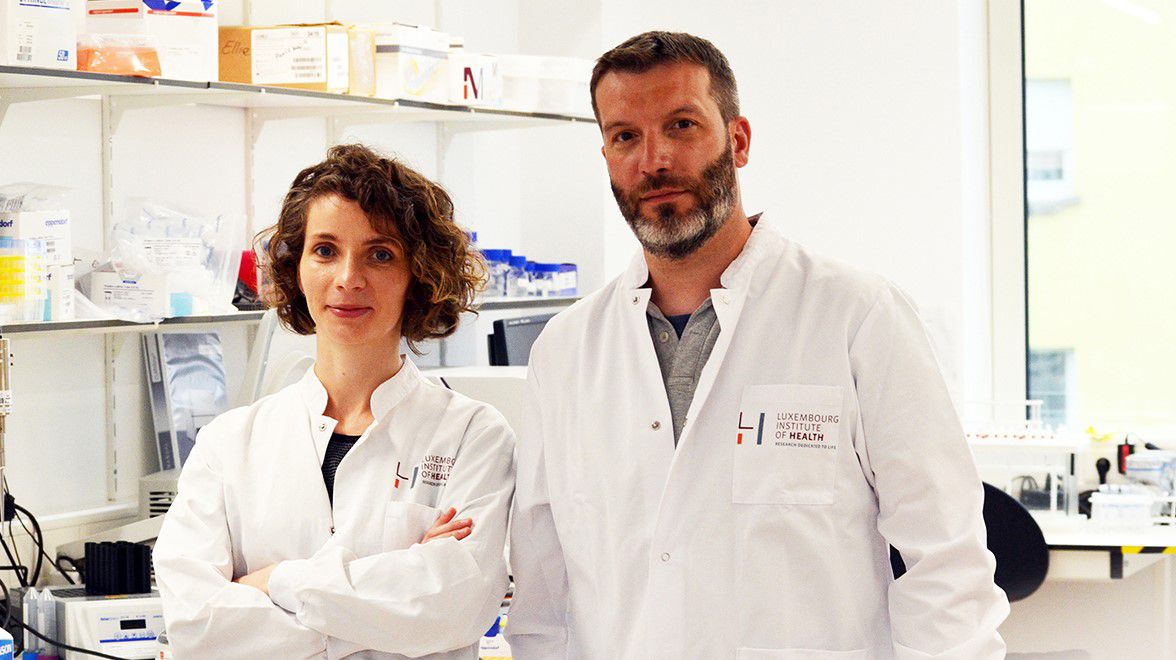
In a recent review, Dr Andy Chevigné and Dr Martyna Szpakowska, from the
Immuno-Pharmacology and Interactomics research group at the LIH Department of Infection and Immunity, recapitulated the implication of these alternative receptors in opioid-related disorders and discussed their unconventional biology to provide an overview of their established and emerging roles in pharmacology in the context of pain management, as well as their clinical relevance as alternative targets to overcome the hurdles of chronic opioid use.
The article describes how despite the discrepancies that led them to be qualified as atypical opioid receptors, there is leading pre-clinical evidence that this class of receptors bind opioid peptides selectively and are able to impact opioid-related phenotypes directly, including pain perception and anxiety, which supports their role as opioid receptors. However, these receptors also have other, non-opioid related functions, such as vasodilation or excitatory neurotransmission among others. The group notes that the potential side effects associated with atypical opioid receptor inhibition or potentiation should therefore be considered, based on both their primary functions and opioid-related behaviours.
“While targeting atypical opioid receptors with specific modulators may appear as a promising new therapeutic avenue, there is only scarce knowledge about some of these receptors’ implication in opioid-related disorders and often limited pharmacological tools available,” explains Christie Palmer, PhD student in the group and first author. “Drugs targeting atypical opioid receptors have shown efficacy in different models and opened up new and unanticipated avenues for drug development, relying on molecules with completely different modes of action and pharmacology than classical opioids. Opioid drugs with weak activity on atypical opioid receptors could also yield a higher benefit/risk ratio.”
Many atypical opioid receptors have been evaluated in the context of pain, anxiety, memory or other opioid-related phenotypes to some extent and there is strong preclinical evidence for their relevance as an alternative means to modulate the opioid machinery. While the opioid receptor family is currently restricted to four receptors, the proposition of a subfamily of atypical opioid receptors allows an extended overview of the possible actors involved in opioid-related disorders. The group argues that following their extensive characterisation, exploiting their breadth of variety may offer new therapeutic opportunities in direct or combined therapies to hopefully broaden and improve the opioid-associated pharmacopoeia.